Health is Social: The Future of Care in Singapore
ETHOS Issue 26, Nov 2023

In his latest Netflix documentary “Live to 100”, author and longevity expert Dan Buettner added Singapore as a sixth ‘Blue Zone’: a region in the world with residents who are known to live long and healthy lives. In his 2020 master class at the Global Wellness Summit,1 Buettner had argued that “the big epiphany of all these Blue Zones is that long-lasting health is very rarely successfully pursued; it ensues”. It is not genetics or willpower that boosts longevity in Blue Zones. It is a lifestyle. Then came Singapore, a Blue Zone that has been engineered, instead of emerging organically like the first five.
Singapore’s life expectancy at birth has been increasing and the number of centenarians has more than doubled from 700 in 2010 to 1,500 in 2020. Its healthy longevity has come from its history, culture and tradition. It has been brought about over time because of its excellent access to healthy food, good healthcare, excellent public infrastructure and social practices that mitigate loneliness, such as intergenerational gatherings. In his documentary, Buettner cited Kampung Admiralty as a feat of engineered health: it houses an indoor park, amenities, apartments, healthcare facilities, and eldercare and preschool centres next to each other.
Singapore leads the world on the health-related Sustainable Development Goals, according to research published in The Lancet in 2017 and part of the Global Burden of Diseases Study. The 2019 edition of the Study reported Singaporeans as living longest in the world, with a life expectancy at birth of 84.9 years and a Healthy Life Expectancy of 73.9 years, with the lowest Disability-Adjusted Life Years (DALY) of 15,045 per 100,000 population. The study also indicated that 35% of our DALY burden could potentially be reduced by early intervention on risk factors contributed by our lifestyles.
With the launch of Healthier SG, Singapore embarks on the largest ever transformation of our care system. We are encouraging residents to enrol with their primary care doctor and establish health plans to keep them well. This is an important first step towards the health of our population. Given that 80% of our total disease burden is from chronic diseases, Preventive Care is the bedrock of our Population Health Strategy.
HEALTH IS FOR ALL
Population Health is not just about better outcomes for individuals but the distribution of those outcomes. Health is not just for the healthy or activated or those who access care. Health is for all. Health is not just for those we can see but those we cannot see. Population Health moves us from the “Story of Me” to the “Story of Us”. In doing so, we expose our vulnerabilities as a population.
Singapore has done well in addressing the social determinants of health like education, transportation, sanitation, housing and so on. With ageing, we see “new” social drivers of health, with an increase in prevalence of dementia, disabilities, frailty, and social isolation. In our centres of healthcare, we often fail to reach those we do not see until they arrive in crisis at our emergency departments. We must do better if we are to change healthcare. Our hospitals are filling up and patients are coming in more ill and with more complex conditions. There are more long stayers. They decondition during their prolonged hospital stay and most are unfit for discharge because they have greater care needs that their homes and communities cannot support. Are more beds then the solution?
The Emotional Side to Activating Senior Health
A community nurse told the story of how TOUCH Community Services sought to encourage more seniors to keep fit by collaborating with ActiveSG to offer weekly aqua aerobics for the seniors. While this seemed like a great idea, not all the seniors owned swimwear. So TOUCH staff worked with donors to sponsor swimwear for the seniors and organised a shopping trip for the seniors to buy swimwear of their choice. This incentive, coupled with encouragement from TOUCH staff and friends, motivated more seniors to sign up for aqua aerobics. They also paired up with one another as buddies to keep a lookout for one another during the sessions. Soon, word of mouth on the positive experience and peer support led to the aqua aerobics class being oversubscribed with a waiting list.
Reflecting on this amazing story of health activation, I suspect that there were deeper feelings at work. Having or buying a swimwear may nudge the early adopters. However, it might not have changed the minds of those who felt vulnerable swimming or wearing swimwear; be it due to their scars from an operation, skin conditions, or anxieties about their body image. But the opportunity to go along with a buddy and as a group let them see each other’s vulnerabilities and therefore gain courage to participate together.

HEALTHCARE ALONE IS NOT ENOUGH
If we look at healthcare as a pipe, we admit and discharge, and we diagnose and treat. We look at healthcare from an efficiency lens because we want throughput and are obsessed with waiting times and bed occupancy. We were once a young population and a young country. The focus was on the iron triangle of Healthcare—Access, Quality and Cost. Hence, we centralised volume to improve quality, especially where expertise and resource was scarce, and to keep costs down. This saw the development of hospitals and specialty centres as highly efficient and specialised centres of excellence.
In the past two to three decades, we introduced quality tools like Clinical Practice Improvement, Lean Healthcare (based on Toyota Production System) and Design Thinking to help reduce waste, improve efficiency, drive productivity and ensure a quality experience. These have served us well to ensure the pipe did not burst. When the healthcare pipe leaked due to pressure, we added resources to ensure a stronger pipe with better flow. Incentives were tied to volume to sustain increasing workload and pace
Today, we are no longer a young population, nor do we have the high economic growth needed to flatten the percentage of Gross Domestic Product (GDP) we spend on health and offset the tripling of our national healthcare expenditure over the last decade. Will more of the same old paradigm give us better health and sustainable healthcare? We know that merely expanding or fixing the pipe that burst will not get us there.
HEALTH & SOCIAL CHANGE: THREE PHILOSOPHICAL SHIFTS
Healthier SG and the recently announced Age Well SG represent a new opportunity to change our healthcare paradigm. Age Well SG supports our seniors to age well in their homes and their communities. Singapore is projected to attain ‘super aged status’ when 21% of our population will be aged 65 years and above in 2026. So Age Well SG seeks to improve our living environment, encourage active ageing and support the care needs of our seniors in their homes and communities. We are moving beyond the iron triangle of healthcare to the triple aim of population health.
The Triple Aim of Population Health goes beyond healthcare to achieve health outcomes for our population, improve the care experience across the system, and sustain cost per capita. In recent years, the triple aim has been expanded to the Quintuple Aim to include the wellbeing of our health workforce and health equity.
To transform our current healthcare system to a population health system, I see three core philosophies taking hold:
- Ownership of Health for All
- Relationships to Care Together
- Stewardship to Invest in Health
- Our residents own their health, not just as individuals but as communities. As an engineered blue zone, we can engineer health in our communities and in doing so, activate communities for health.
- Care should shift from transactional care encounters to building trusting care relationships that span the life course. These relationships wrap around care for our residents.
- The stewardship of a population health system requires a mindset shift from Healthcare being a cost to Health being our best investment for the future. The longer game in healthcare sustainability is not just cost containment, but commitment to grow our health as a nation.
|
According to the Ministry of Health (MOH): |
||
|---|---|---|
 |
In 2019, the number of elderly living alone increased to 67,600, up from 47,000 in 2016. This increase represents 11.9% of our elderly population. | |
 |
1,000 attemped suicides. | |
 |
400 reported suicides, with 122 being above 60 years of age. | |
 |
1 in 10 seniors above 60 years of age has dementia. | |
|
According to the National Healthcare Group (NHG): |
||
 |
15% of our elderly residents are living with frailty. | |
|
According to a Department of Statistics Population Census Report: |
||
 |
In 2020, 100,000 residents were unable to perform or had a lot of difficulty performing one basic activity. | |
The impact of ageing on the elderly stirs us because it is also what we can all look forward to in time to come.
Building a Community of Care: Madam Amy’s Story
by J R Karthikeyan, CEO, AWWA Ltd.
Amid the landscape of an ageing population within the Ang Mo Kio vicinity, the collaborative efforts of healthcare institutions and social service agencies are critical in providing holistic care for seniors. With this shared aspiration in mind, AWWA, Tan Tock Seng Hospital (TTSH), National Healthcare Group Polyclinics (NHGP), the Agency for Integrated Care-Silver Generation Office (AIC-SGO), and PanCare Medical Clinic came together to actualise it with Community of Care (CoC).
With CoC, Ang Mo Kio resident Madam Amy’s memory and health issues have not stopped her from participating actively within the community. To build trust and a genuine connection, the team at AWWA initiated befriending visits, and soon learned that Madam Amy was hesitant to seek the medical assistance she required. Working with TTSH’s Community Health Team (CHT) to assess her condition, the team worked out her unique needs and relevant care goals, while respecting her desire to remain independent.
For continued support, the AWWA team conducted regular checks to monitor Madam Amy’s medication administration and vital signs. In addition, they created a personalised visual schedule with her favourite cat photos and voice-recorded reminders to encourage Madam Amy to take her medication on time. The team at PanCare Medical Clinic, which sits within the Ang Mo Kio vicinity, added to the network of support through home consultations, to ensure that her chronic conditions were comprehensively managed.
The community also rallied around Madam Amy, with neighbours and local shop owners keeping a lookout for her and her brother staying in close contact to ensure her wellbeing.
The CoC model of collaborative care reflects a deep commitment to supporting seniors through strong partnerships so that they are empowered to take control of their health, thrive, and age well throughout their golden years.

We are building a Community of Care (CoC) in every neighbourhood to bring Healthier SG and Age Well SG to our population. Every CoC is anchored by an Active Ageing Centre (AAC) catering to elderly residents in that neighbourhood. By bringing together national and social agencies, family doctors, community health teams and residents, CoCs can bridge health and social care for the elderly in their communities and empower residents to proactively manage their health and embrace healthier living.
Our residents own their health, not just as individuals but as communities.
BUILDING CAPABILITIES FOR HEALTH AND SOCIAL CHANGE
The Centre for Healthcare Innovation’s (CHI) Health & Social Change Academy was launched on 28 July 2023 by Minister for Health Ong Ye Kung.
It aims to build the capabilities of health and social care professionals to work together in developing programmes and initiatives to engage the population on health issues collaboratively. The Academy is supported by strategic partners from across agencies, academia, healthcare, and community partners, including the AWWA, Care Corner Singapore, Methodist Welfare Services (MWS), and TOUCH Community Services. These partnerships and programmes will grow as it expands as a movement to launch initiatives for health and social change.
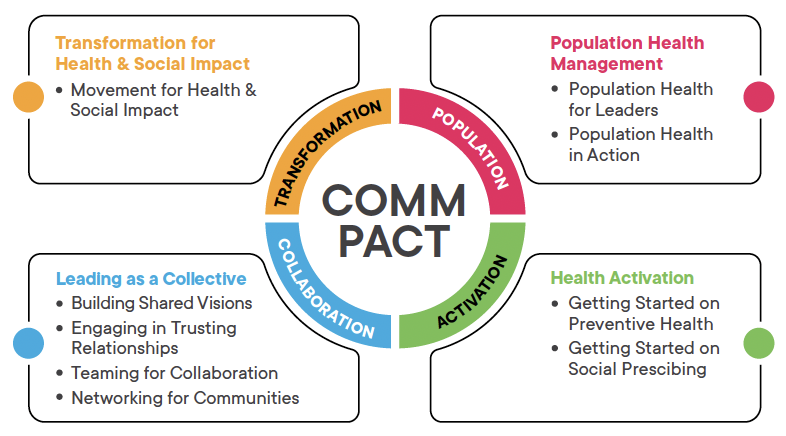
The academy features four strategic programmes to build Communities of Care through PACT—Population Health Management, Health Activation, Leading as a Collective and Transformation for Health & Social Impact.

The Academy will host more than 30 local and international experts from academia, health and social care, and government agencies under the CHI Co-Learning Network. The Academy’s curriculum is designed around the premise that building healthier, happier communities requires a collective commitment and effort. Hence, it aims to nurture the environment for various stakeholders to come together to understand one another’s roles in the community, learn new skills and concepts, and take collective action to design care that will keep our people and future generations healthier and happier.
BUILDING DIGITAL HEALTH COMMUNITIES
Alongside the academy, a digital sandbox called the Digital CoC Playground has been set up to facilitate collaborations, specifically on digital solutions that will more easily engage and activate residents to adopt healthy behaviour. These innovative solutions will be introduced and tested in real-world settings and, where appropriate, be scaled up to keep residents healthy and engaged.
The Digital CoC Playground will enable key stakeholders in the CoCs to identify and discuss everyday health and social care issues that residents face and develop personalised digital solutions to meet their needs. When community partners bring their problem statements into the Playground, CHI will help match them with like-minded organisations, sponsors, technology experts and funders to pursue the creation of a digital CoC solution together. This collaborative Playground will serve as a test bed for the digital solutions to be piloted in the community before they are adopted or expanded to benefit more residents. Such digital solutions will complement existing programmes and services at a physical CoC. They will address three key aspects: Care to follow the Resident; Outreach to a wider Resident Population; and Integration to enable Resident-centricity so that they may own their health with the care and support needed.
By leveraging digital technology, we aim to overcome the limitations associated with resource-intensive care support work and introduce new ways to serve and empower a more significant number of residents towards healthy living that may not be possible with physical CoCs alone. Our elderly accounts for 20% or more of residents living in established neighbourhoods. A place-based care strategy works best for the elderly, while the young seniors above 50 years of age and the younger population are more mobile. The Digital CoC presents opportunities to engage and activate more residents to adopt healthy behaviours, regardless of their age, health status and location.
By providing care where residents live, work and play, we anticipate that these Digital CoCs can better integrate health-social initiatives that bring about happier and healthier communities across various settings, including the neighbourhood, schools, and workplaces. This integrated approach will form a comprehensive support system that addresses residents’ diverse needs and aspirations.
Building healthier, happier communities requires a collective commitement and effort.
DEEPENING THE RELATIONSHIPS THAT MATTER
As we organise for Health & Social Change, we need a collective leadership beyond the walls of our healthcare system. Working closely with partners and residents, we can transform our future Health & Social Care to ensure that Health is for All.
Working in the National Healthcare Group, I am immensely proud of our vision of Adding Years of Healthy Life. It is not enough that we add Years to Life: we must also add Life to our Years. This is an ambitious vision, but Singapore can become a deep Blue Zone: not just living longer lives, but living better, and more fully, together.
NOTE
- See: Meredith Clark, “What Are Blue Zones and Why Do Some Suggest They Are the Secret to Living Longer?” https://www.independent.co.uk/life-style/health-and-families/blue-zones-netflix-diet-documentary-b2408185.html..

